How Comatose Patient Transfer Equipment Supports ICU Transport
Comatose patient transfer equipment sits at the heart of every safe ICU move. It keeps ventilation stable. It protects circulation. It preserves sedation and monitoring between beds, vehicles, and skies. Yet gear alone does not save a life. Timing, protocols, and trained hands turn hardware into an ICU without walls. In this story, TKP Medical Assistance lifts the curtain on the tools we trust and the steps we refuse to skip.
How Comatose Patient Transfer Equipment Keeps ICU-Level Care Moving
When a patient is comatose, time and stability matter more than anything else. Our clinicians build each mission around equipment and procedures that preserve airway security, ventilation, circulation, and sedation from the first bedside touch to the final handover. The goal is simple: zero gaps in care, even when the environment changes from ward to ambulance, ambulance to aircraft, or aircraft to rail.
We start with structure, not improvisation. Before departure, our team completes a focused ICU assessment, validates sedation and analgesia plans, and maps oxygen and electrical needs across the whole route. We calculate battery life, confirm oxygen reserves with headroom for delays, and prepare backup devices. During transport we keep medication infusions running, apply invasive monitoring when indicated, and document every setting so receiving clinicians can verify and continue. In practice, comatose patient transfer equipment is only as effective as the protocol behind it – so we tie hardware to checklists, escalation triggers, and clear communication.
The Toolkit That Makes Stability Possible
For air ambulance ICU transport and complex ground legs, we deploy ventilators that support pressure and volume modes suitable for fragile lungs; multi-parameter monitors with invasive lines for reliable trending; and infusion and syringe pumps that maintain exact sedation and vasopressor doses. Robust stretcher-litter interfaces lock to aircraft and ambulance mounts, limiting motion and protecting lines. When needed, we run advanced life-support systems – ECMO or IABP – under the supervision of intensive-care physicians and flight-trained nurses. Immobilization devices and careful lift techniques help secure the airway and reduce shear injury risk. Redundant power and oxygen pathways stand ready if a primary source fails. In short, comatose patient transfer equipment is integrated, standardized, and chosen for continuity rather than convenience.
From the Plateau to the Capital: A Mission That Tested Every Detail
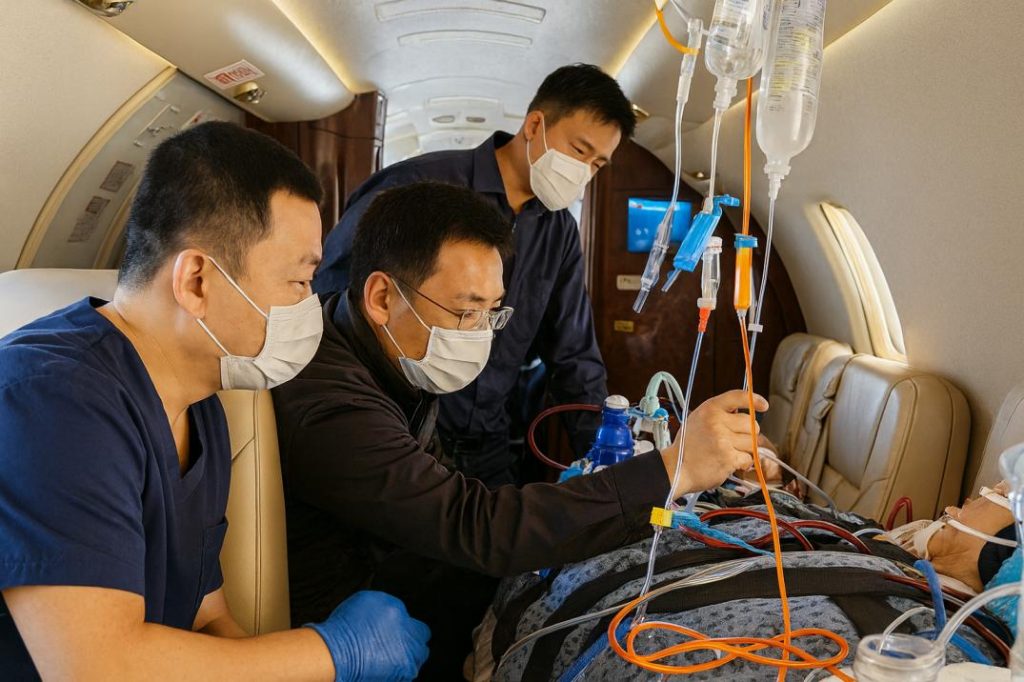
On January 6, 2025, we coordinated a time-critical transfer from Lhasa → Chengdu → Beijing by air ambulance. The patient had severe pneumonia with respiratory failure and was comatose. Altitude and hypoxia shaped every choice we made. A charter flight – arranged by the employer for their staff – created a safe window for departure. At the bedside in Lhasa, we adjusted ventilator settings and hemodynamic support to pre-optimize oxygenation before the first move. Around 3,000 meters above sea level, we performed final checks, secured lines and devices, and verified backup oxygen and power.
Inside the cabin, the physiology of the plateau demanded precision. Barometric pressure reduces oxygen partial pressure; even small ventilator changes can shift gas exchange. Our approach combined altitude-aware ventilator strategies with conservative titration and tight monitoring. The cabin crew coordinated with our clinicians so respiratory and circulatory support could be implemented smoothly in a hypoxic environment. Above the clouds, continuous observation – rhythm, oxygenation, perfusion – turned uncertainty into manageable risk. Here, comatose patient transfer equipment did more than travel with the patient; it preserved the patient’s stability.
Key Safeguards We Applied
- Pre-transport ICU assessment tailored to altitude risk and flight profile
- Ventilation and circulation plans with altitude-aware targets and backups
- Continuous monitoring and documented handover at each segment
This mission also illustrates a broader point: standardized equipment and rehearsed workflows shorten handovers and make complex, multi-leg itineraries predictable. That reliability is why families, employers, and insurers trust us with bedridden patient transport that must cross regions and borders without compromising ICU standards.

Why TKP Medical Assistance Delivers Across Borders
TKP Medical Assistance is a comprehensive, cross-regional medical transport organization included in the National Health Commission’s foreign emergency rescue network unit. Since our founding in 2001, we have handled 71,000 pieces of global information and 10,000 operational cases. Our network covers the world, and we work closely with airlines, general aviation companies, and major domestic and foreign insurance companies. Those relationships translate into faster clearances, consistent aircraft availability, and the ability to match comatose patient transfer equipment to the realities of a specific route.
We recommend the transport mode that fits the clinical picture and the itinerary – not the other way around:
• Air Ambulance & ICU Transfers. Aircraft equipped with ICU-grade monitoring, ventilators, and life support. Missions are staffed by intensive-care physicians and flight-trained nurses to keep critically ill patients stable at altitude.
• Commercial Stretcher Transfers. With airline approval, we arrange a dedicated stretcher compartment on scheduled flights. Medical escorts accompany the journey – a cost-effective choice for stable, bedridden patients needing cross-border movement.
• Rail-Based Medical Transfers. Coordinated high-speed rail segments with ambulance pick-up and drop-off. Ideal when flight is unsuitable, including neonatal or post-surgical cases requiring continuous monitoring during non-flight legs.
Across these modes, our standardization is deliberate. The same ventilators, monitors, infusion pumps, and mounting systems appear from one segment to the next. Settings are synchronized, alarms are harmonized, and documentation travels with the patient. This alignment minimizes error, reduces handover time, and supports the clinical calm that a comatose patient requires. It is also central to our cross-border medical evacuation services, where a single itinerary may involve multiple jurisdictions, airframes, and clinical teams.
For families and case managers, predictability is peace of mind. We offer clear route planning, transparent equipment lists, and staffing profiles that match acuity. We also prepare contingencies: diversions for weather, backup oxygen calculations, auxiliary power, and alternate receiving facilities. The result is a transport plan that holds firm when the day refuses to cooperate.
If you are comparing providers, ask how your partner thinks about comatose patient transfer equipment: Is it interchangeable gear, or is it part of an integrated system with training, checklists, and redundant pathways? At TKP Medical Assistance, our answer is built into how we work. The hardware matters. The choreography around it matters just as much.
Ready to Move Safely?
Contact TKP Medical Assistance for a rapid, no-obligation case review. We will analyze route options, define the equipment and staffing profile, and give you a clear plan to relocate your ICU patient with confidence – whether by air ambulance, commercial stretcher on an international medical flight, or coordinated rail-and-road.
Submit Your Request
Recent Posts
Tags
- Air Ambulance
- Bedside To Bedside
- Cross Border Aid
- Emergency Evacuation
- Global Medical Rescue
- How can I ensure the patient's stability while in the air?
- How do I request an air medical transport?
- How is it different from an air ambulance
- how to activate emergency aircraft service
- how to request an air ambulance
- Is air medical transport safe
- Is international transport possible
- Medical Rescue
- Medical Transport
- Patient Repatriation
- Remote Rescue
- Seamless Coordination
- Telemedicine Support
- Tourists And Expats Medical Escort
- What are the benefits of a cross-border medical transfer
- What are the different types of transfers
- What are typical use cases
- What documents do I need to prepare for a transfer?
- What does high-speed rail patient transfer stands for
- What is air ambulance
- What is air medical transport?
- What is cross-border medical transfer
- What is emergency aircraft
- what is high-speed rail patient transfer
- What is medical charter flight
- what is neonatal ICU transfer
- What is patient air transfer
- What medical equipment is available on board the aircraft
- What situations shouldn't use air medical transport?
- What types of air ambulance are there?
- What types of air ambulance exist
- What's the difference between international and domestic transfers?
- what’s the difference between air medical transport and regular ambulance?
- When is emergency air transport necessary
- Which patients require air medical transport?
- who is included in the medical team
- who needs an air ambulance






