How Technology Improves Emergency Comatose Patient Transfer Safety
Emergency Comatose Patient Transfer demands calm action under pressure, precise teamwork, and tools that never blink. At TKP Medical Assistance, we use technology to narrow the risk window and keep care truly bedside-to-bedside. Clinical skill matters; so does digital coordination. When both align, every minute – and every meter of altitude – tilts in the patient’s favor.

From Plateau to Tertiary Care: Creating a Safe Corridor
High-acuity cases do not wait for perfect weather or easy geography. On January 6, 2025, our team conducted an air-ambulance mission Lhasa → Chengdu → Beijing for a patient with severe pneumonia, respiratory failure, and a comatose presentation. The plateau environment is unforgiving. Oxygen is thin, temperatures swing, and small delays magnify clinical risk.
We began by building a safe transport window at the ward in Lhasa. Ventilator settings were tuned for altitude; sedation and hemodynamic targets were stabilized; lines and tubes were secured for movement. Before lift-off, at roughly 3,000 meters, the team ran final checks on ventilation, perfusion, and cabin oxygen delivery. Once airborne, the focus shifted to high-frequency observation: tidal volumes, end-tidal CO₂, SpO₂ trends, and vasoactive requirements. The cabin crew and medical team moved in lockstep, executing each transfer step – bed to stretcher, stretcher to aircraft, aircraft to ICU – without jeopardizing airway integrity or circulatory stability.
What preserves safety in Emergency Comatose Patient Transfer is not a single gadget but a connected stack. Digital flight planning syncs with weather and altitude data. Bedside checklists are matched to the aircraft cabin profile. Handoff packets mirror the receiving ICU’s expectations. When each element talks to the next, a hostile route becomes a controlled corridor – an essential principle of high-altitude patient transport safety.
Case Snapshot: Lhasa → Chengdu → Beijing
- Mode: Air ambulance, with charter coordination provided by the employer
- Condition: Severe pneumonia, respiratory failure, comatose state
- Pre-Transport: On-site treatment adjustment in Lhasa to open the transport window
- In-Flight: Continuous monitoring of oxygenation, ventilation, and circulation in a hypoxic cabin
- Process Flow: Ward → Ambulance → Aircraft → ICU, safeguarding airway and lines at each step
The TKP Safety Stack: Systems That Protect Every Minute
Technology should simplify complexity, not add to it. Our workflow for Emergency Comatose Patient Transfer integrates software, devices, and human protocols into one repeatable system.
Dynamic Route Intelligence
Air routes are planned to shorten flight time and reduce altitude stress. We use strategically selected airports – including those with limited infrastructure – to connect remote or underserved origins with tertiary centers. Optimized pathways trim minutes without trading away safety.
Operations Center With Live Oversight
A 24/7 coordination team tracks aircraft position, weather, and clinical telemetry in real time. If conditions change, routes and handoffs adjust instantly. This constant watch reduces avoidable delays and protects clinical stability during transfers.
Bedside-To-Bedside Protocols
Standardized bundles guide airway protection, sedation, ventilation targets, and pressure-injury prevention across ambulance, aircraft, and ICU. Using one shared playbook lowers the risk of handoff errors – the hidden culprit in many adverse events.
Cross-Border Enablement
International transfers often falter on paperwork rather than medicine. We coordinate with medical institutions and embassies to secure documentation and clearances, a must for cross-border air ambulance services where bureaucracy can erode precious time.
Data-Driven Go/No-Go Readiness
Pre-transport scoring, oxygen reserve planning, and equipment right-sizing keep the team honest about risk. When thresholds are clear, decisions are faster and safer.
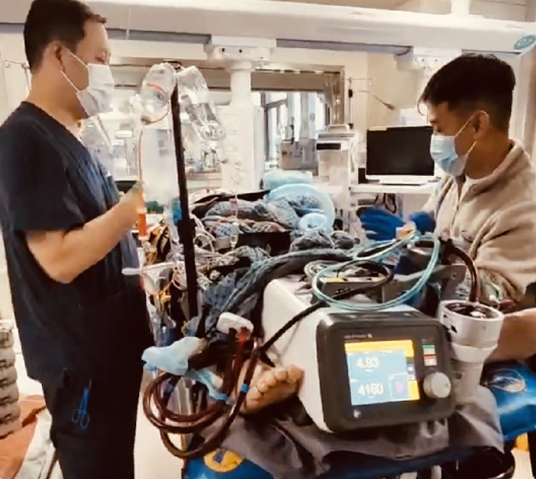
Life-Sustaining Systems In Transit
We operate ECMO, IABP, advanced ventilators, and vasoactive infusions throughout the journey, including international flight segments. Teams are trained for constrained spaces and variable cabin pressures. Where clinically appropriate, this capability extends to critically ill neonates. The aim is continuity: perfusion and gas exchange maintained without interruption until the receiving ICU assumes care.
Why This Stack Matters
- Fewer Delays: Optimized routes and real-time coordination reduce exposure to hypoxia and instability.
- Cleaner Handoffs: Shared data and checklists keep all teams aligned on the same targets.
- Controlled Variance: Standardized protocols travel with the patient, limiting unpredictable swings in care.
Value For Hospitals, Employers, And Families
Hospitals are juggling bed capacity, variable ground links, and uneven documentation flows. Employers carry the weight of duty-of-care decisions across borders. Families want transparency and compassionate updates. Technology alone cannot answer these needs; technology deployed through disciplined process can.
For hospitals, the win is time compression to definitive care. Real-time routing, rapid clearances, and altitude-aware ventilation strategies shorten the period in which the patient is most vulnerable. With synchronized handoffs, the receiving ICU gets coherent data and stable patients – not a reset button.
For employers, value shows up as predictable logistics and clear communication. We outline a corridor from origin to destination, explain contingencies, and maintain updates at each segment. That clarity keeps obligations on track and reduces costly last-minute pivots.
For families, confidence grows from visible coordination. They see the sequence – ward, ambulance, aircraft, ICU – and hear how the targets are being met along the way. The journey feels guided, not improvised.
In the Lhasa mission, every leg reinforced the last. The ventilatory targets held. Vasoactive support remained steady. Positioning strategies were preserved through each handoff. The chain did not break, and that is the standard we aim to repeat in every Emergency Comatose Patient Transfer: speed without chaos, movement without compromise.
Final Words
If your hospital, company, or family needs high-acuity transfer – especially from remote or high-altitude regions – contact TKP Medical Assistance. We will assess the case, align route and resources, and orchestrate a bedside-to-bedside plan anchored in technology and clinical discipline. When minutes matter most, we build safe corridors to definitive care.
Submit Your Request
Recent Posts
Tags
- Air Ambulance
- Bedside To Bedside
- Cross Border Aid
- Emergency Evacuation
- Global Medical Rescue
- How can I ensure the patient's stability while in the air?
- How do I request an air medical transport?
- How is it different from an air ambulance
- how to activate emergency aircraft service
- how to request an air ambulance
- Is air medical transport safe
- Is international transport possible
- Medical Rescue
- Medical Transport
- Patient Repatriation
- Remote Rescue
- Seamless Coordination
- Telemedicine Support
- Tourists And Expats Medical Escort
- What are the benefits of a cross-border medical transfer
- What are the different types of transfers
- What are typical use cases
- What documents do I need to prepare for a transfer?
- What does high-speed rail patient transfer stands for
- What is air ambulance
- What is air medical transport?
- What is cross-border medical transfer
- What is emergency aircraft
- what is high-speed rail patient transfer
- What is medical charter flight
- what is neonatal ICU transfer
- What is patient air transfer
- What medical equipment is available on board the aircraft
- What situations shouldn't use air medical transport?
- What types of air ambulance are there?
- What types of air ambulance exist
- What's the difference between international and domestic transfers?
- what’s the difference between air medical transport and regular ambulance?
- When is emergency air transport necessary
- Which patients require air medical transport?
- who is included in the medical team
- who needs an air ambulance






